Information on this site should not be considered to be medical advise and we are not physicians, it is provided to stimulate conversation between you and your Doctor. Before taking or doing anything herein, please consult your Physician.
MIT Study Shows:
Fasting boosts stem cells’ regenerative capacity
News from MIT
Anne Trafton | MIT News Office
May 3, 2018
OK, for some of you here is the short version:
A 24 hour fast can potentially cause your stem cells to double their regenerative capacity, at least if your cells respond like the test mice did. This can be extremely helpful if your bowels aren't working as well as you'd like. [This Report deals with intestinal cells, however reports indicate that stem cells are also responsible for joint repair and could have a regenerative effect upon cartilage in your joints and reduction of joint pain, and possibly are a significant repair system for many areas in the body.].
As people age, their intestinal stem cells begin to lose their ability to regenerate. These stem cells are the source for all new intestinal cells, so this decline can make it more difficult to recover from gastrointestinal infections or other conditions that affect the intestine.
This age-related loss of stem cell function can be reversed by a 24-hour fast, according to a new study from MIT biologists. The researchers found that fasting dramatically improves stem cells’ ability to regenerate, in both aged and young mice.
If you decide you'd like to try it, there is a Fasting Drink recipe at the end that will completely kill your appetite for hours, if not days.
As people age, their intestinal stem cells begin to lose their ability to regenerate. These stem cells are the source for all new intestinal cells, so this decline can make it more difficult to recover from gastrointestinal infections or other conditions that affect the intestine.
This age-related loss of stem cell function can be reversed by a 24-hour fast, according to a new study from MIT biologists. The researchers found that fasting dramatically improves stem cells’ ability to regenerate, in both aged and young mice.
In fasting mice, cells begin breaking down fatty acids instead of glucose, a change that stimulates the stem cells to become more regenerative. The researchers found that they could also boost regeneration with a molecule that activates the same metabolic switch. Such an intervention could potentially help older people recovering from GI infections or cancer patients undergoing chemotherapy, the researchers say.
“Fasting has many effects in the intestine, which include boosting regeneration as well as potential uses in any type of ailment that impinges on the intestine, such as infections or cancers,” says Omer Yilmaz, an MIT assistant professor of biology, a member of the Koch Institute for Integrative Cancer Research, and one of the senior authors of the study. “Understanding how fasting improves overall health, including the role of adult stem cells in intestinal regeneration, in repair, and in aging, is a fundamental interest of my laboratory.”
David Sabatini, an MIT professor of biology and member of the Whitehead Institute for Biomedical Research and the Koch Institute, is also a senior author of the paper, which appears in the May 3 issue of Cell Stem Cell.
“This study provided evidence that fasting induces a metabolic switch in the intestinal stem cells, from utilizing carbohydrates to burning fat,” Sabatini says. “Interestingly, switching these cells to fatty acid oxidation enhanced their function significantly. Pharmacological targeting of this pathway may provide a therapeutic opportunity to improve tissue homeostasis in age-associated pathologies.”
The paper’s lead authors are Whitehead Institute postdoc Maria Mihaylova and Koch Institute postdoc Chia-Wei Cheng.
Boosting regeneration
For many decades, scientists have known that low caloric intake is linked with enhanced longevity in humans and other organisms. Yilmaz and his colleagues were interested in exploring how fasting exerts its effects at the molecular level, specifically in the intestine.
Intestinal stem cells are responsible for maintaining the lining of the intestine, which typically renews itself every five days. When an injury or infection occurs, stem cells are key to repairing any damage. As people age, the regenerative abilities of these intestinal stem cells decline, so it takes longer for the intestine to recover.
“Intestinal stem cells are the workhorses of the intestine that give rise to more stem cells and to all of the various differentiated cell types of the intestine. Notably, during aging, intestinal stem function declines, which impairs the ability of the intestine to repair itself after damage,” Yilmaz says. “In this line of investigation, we focused on understanding how a 24-hour fast enhances the function of young and old intestinal stem cells.”
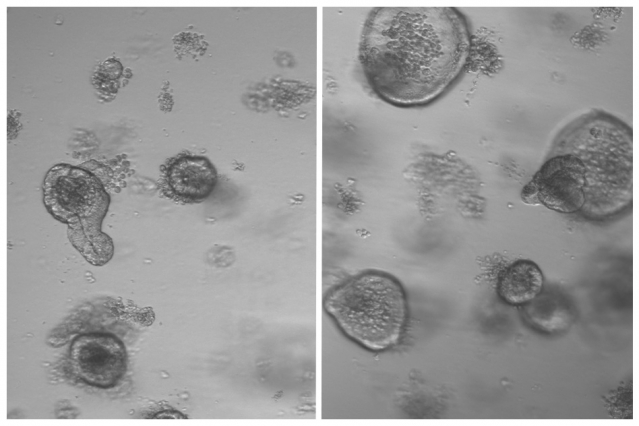
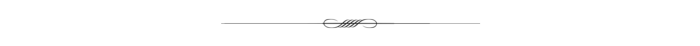
After mice fasted for 24 hours, the researchers removed intestinal stem cells and grew them in a culture dish, allowing them to determine whether the cells can give rise to “mini-intestines” known as organoids.
The researchers found that stem cells from the fasting mice doubled their regenerative capacity.
“It was very obvious that fasting had this really immense effect on the ability of intestinal crypts to form more organoids, which is stem-cell-driven,” Mihaylova says. “This was something that we saw in both the young mice and the aged mice, and we really wanted to understand the molecular mechanisms driving this.”
Metabolic switch
Further studies, including sequencing the messenger RNA of stem cells from the mice that fasted, revealed that fasting induces cells to switch from their usual metabolism, which burns carbohydrates such as sugars, to metabolizing fatty acids. This switch occurs through the activation of transcription factors called PPARs, which turn on many genes that are involved in metabolizing fatty acids.
The researchers found that if they turned off this pathway, fasting could no longer boost regeneration. They now plan to study how this metabolic switch provokes stem cells to enhance their regenerative abilities.
They also found that they could reproduce the beneficial effects of fasting by treating mice with a molecule that mimics the effects of PPARs. “That was also very surprising,” Cheng says. “Just activating one metabolic pathway is sufficient to reverse certain age phenotypes.”
Jared Rutter, a professor of biochemistry at the University of Utah School of Medicine, described the findings as “interesting and important.”
“This paper shows that fasting causes a metabolic change in the stem cells that reside in this organ and thereby changes their behavior to promote more cell division. In a beautiful set of experiments, the authors subvert the system by causing those metabolic changes without fasting and see similar effects,” says Rutter, who was not involved in the research. “This work fits into a rapidly growing field that is demonstrating that nutrition and metabolism has profound effects on the behavior of cells and this can predispose for human disease.”
The findings suggest that drug treatment could stimulate regeneration without requiring patients to fast, which is difficult for most people. One group that could benefit from such treatment is cancer patients who are receiving chemotherapy, which often harms intestinal cells. It could also benefit older people who experience intestinal infections or other gastrointestinal disorders that can damage the lining of the intestine.
The researchers plan to explore the potential effectiveness of such treatments, and they also hope to study whether fasting affects regenerative abilities in stem cells in other types of tissue.
The research was funded by the National Institutes of Health, the V Foundation, a Sidney Kimmel Scholar Award, a Pew-Stewart Trust Scholar Award, the MIT Stem Cell Initiative through Fondation MIT, the Koch Institute Frontier Research Program through the Kathy and Curt Marble Cancer Research Fund, the American Federation of Aging Research, the Damon Runyon Cancer Research Foundation, the Robert Black Charitable Foundation, a Koch Institute Ludwig Postdoctoral Fellowship, a Glenn/AFAR Breakthroughs in Gerontology Award, and the Howard Hughes Medical Institute.
As people age, their intestinal stem cells begin to lose their ability to regenerate. These stem cells are the source for all new intestinal cells, so this decline can make it more difficult to recover from gastrointestinal infections or other conditions that affect the intestine.
This age-related loss of stem cell function can be reversed by a 24-hour fast, according to a new study from MIT biologists. The researchers found that fasting dramatically improves stem cells’ ability to regenerate, in both aged and young mice.
In fasting mice, cells begin breaking down fatty acids instead of glucose, a change that stimulates the stem cells to become more regenerative. The researchers found that they could also boost regeneration with a molecule that activates the same metabolic switch. Such an intervention could potentially help older people recovering from GI infections or cancer patients undergoing chemotherapy, the researchers say.
“Fasting has many effects in the intestine, which include boosting regeneration as well as potential uses in any type of ailment that impinges on the intestine, such as infections or cancers,” says Omer Yilmaz, an MIT assistant professor of biology, a member of the Koch Institute for Integrative Cancer Research, and one of the senior authors of the study. “Understanding how fasting improves overall health, including the role of adult stem cells in intestinal regeneration, in repair, and in aging, is a fundamental interest of my laboratory.”
David Sabatini, an MIT professor of biology and member of the Whitehead Institute for Biomedical Research and the Koch Institute, is also a senior author of the paper, which appears in the May 3 issue of Cell Stem Cell.
“This study provided evidence that fasting induces a metabolic switch in the intestinal stem cells, from utilizing carbohydrates to burning fat,” Sabatini says. “Interestingly, switching these cells to fatty acid oxidation enhanced their function significantly. Pharmacological targeting of this pathway may provide a therapeutic opportunity to improve tissue homeostasis in age-associated pathologies.”
The paper’s lead authors are Whitehead Institute postdoc Maria Mihaylova and Koch Institute postdoc Chia-Wei Cheng.
Fasting Drink
This drink will completely kill your appetite for many hours. In other words, you can fast with virtually NO willpower if you drink this first. I was able to fast for 5 days with absolutely NO willpower other than deciding that I would drink this drink before eating anything. There were many times I'd be drinking this while standing in front of the refrigerator trying to decide what I was going to eat when I finished the drink, only to find I'd completely lost my appetite. This would last for perhaps 5 or 6 hours or more. I was amazed. Your experience may vary, but it's worth a try. I've spoken to people who were taking drugs (such as Nexium, Prilosec, Prevacid, Protonix or Aciphex) for acid reflux who found that when they had been taking a pill every day, after fasting, could go 5 to 7 days between pills with no reflux. Your experience may vary and speak with your doctor before trying this or changing your medication.
The one thing that I might mention. Many things contain minute amounts of chemicals and preservatives. These are said to become concentrated in your stored fat. As you fast, your body begins to break down and digest this fat, and while that is great for loosing weight, the chemicals and preservatives often come out in concentrated amounts and can cause a whopper of a headache, but it does go away. You might consider taking an asprin or pain killer when you first notice it.
Be sure to check with yor Doctor before trying anything based upon any information you may find on this site. This is a recipe provided by a Doctor with the Kaiser Permanente Hawaii Kai Clinic.
Juice of half a fresh lemon (FRESH, Not from a container)
2 T. Pure Maple Syrup
8 to 10 ounces of water (hot or cold)
1/8 t. red cayenne pepper
The red pepper completely ruins the otherwise maple lemonade flavor. I strongly suggest don't add it to the drink, but rather wash it down with your first sip.
In related news, scientists have mapped and identified almost 8,000 different strains of bacteria in the human intestinal tract.
See "A comprehensive catalogue of human digestive tract bacteria"
Researchers identify nearly 8,000 strains of bacteria, while also clarifying their genetic and metabolic context.
Anne Trafton | MIT News Office September 2, 2019
The human digestive tract is home to thousands of different strains of bacteria. Many of these are beneficial, while others contribute to health problems such as inflammatory bowel disease. Researchers from MIT and the Broad Institute have now isolated and preserved samples of nearly 8,000 of these strains, while also clarifying their genetic and metabolic context. This data set (BIO-ML), which is available to other researchers who want to use it, should help to shed light on the dynamics of microbial populations in the human gut and may help scientists develop new treatments for a variety of diseases, says Eric Alm, director of MIT’s Center for Microbiome Informatics and Therapeutics and a professor of biological engineering and of civil and environmental engineering at MIT.
“There’s a lot of excitement in the microbiome field because there are associations between these bacteria and health and disease.
For Information on the gut microbiome: How does it affect our health?
Most of us are aware that the bacteria in our gut play an important role in digestion. When the stomach and small intestine are unable to digest certain foods we eat, gut microbes jump in to offer a helping hand, ensuring we get the nutrients we need. In addition, gut bacteria are known to aid the production of certain vitamins - such as vitamins B and K - and play a major role in immune function. But increasingly, researchers are working to find out more about how gut bacteria - particularly the bacteria that is unique to us individually - influence our health and risk of disease. Perhaps most studied is how gut microbiota affects an individual's risk of obesity and other metabolic conditions. [Some researchers speculate that it can also affect allergies, Ceilac Disease, Crohn’s disease, Ulcerative colitis, Irritable bowel syndrome (IBS) (WebMD), Autism, diabetes, heart disease, obesity, anxiety, depression, also may help ease allergy symptoms and help with lactose intolerance and excessive weight gain. Some feel the gut bacteria can be adversely affected by the anoumt of chlorine or chloramine used to sterilize our drinking water as can the small amounts of Glyphosate (Roundup) that are still attached to grain and Genetically Modified plants and vegetables. Apparently some gut bacteria are killed by those trace amounts and they encourage people to be aware of how their drinking water is treated. ]
In detail, the study - conducted by researchers from Cornell University in Ithaca, NY, and King's College London in the UK - found that a certain strain of bacteria - Christensenellaceae minuta - was more common in people with a low body weight, and that the presence of this particular strain is highly influenced by genes.
What is more, introducing this bacteria to the guts of mice caused the animals to gain less weight, indicating the bacteria may reduce or prevent obesity.
Anxiety and Depression
With this in mind, it is perhaps unsurprising that gut bacteria have been associated with a number of mental health problems, including anxiety disorders and depression.
In 2014, for example, a study published in the journal Psychopharmacology found that prebiotics - carbohydrates that boost healthy bacteria in the gut - may be effective for reducing stress and anxiety.
Autism
Autism is estimated to affect 1 in 68 children in the US. While studies have associated environmental factors - such as pollution - and genetics as potential causes of the disorder, researchers are increasingly looking at the role of gut bacteria in its development.
In 2013, a study by researchers from Arizona State University found that children with autism possessed lower levels of three types of gut bacteria - Prevotella, Coprococcus and Veillonellaceae - compared with children free of the condition.
A more recent study from the team found that concentrations of specific chemicals produced by gut bacteria - called metabolites - in fecal samples of children with autism differed to the concentrations found in the fecal samples of children without the disorder.
This led the researchers to hypothesize that gut microbes alter the metabolites associated with communication between the gut and the brain, which interferes with brain function.
Further strengthening the association between gut bacteria and autism is a 2013 study published in Cell that found the bacterium Bacteroides fragilis reduced autism-like symptoms in mice. [See hazards associated with Bacteroides fragilis here ]
See the Full Article here
See also How Can You Improve Your Gut Microbiome?
Read The Case Against Chlorinated Tap Water